Tzioupis, C. & Giannoudis, P. V. Prevalence of long-bone non-unions. Injury 38, S3–S9 (2007).
Calori, G. M., Mazza, E., Colombo, M., Ripamonti, C. & Tagliabue, L. Treatment of long bone non-unions with polytherapy: indications and clinical results. Injury 42, 587–590 (2011).
Zura, R. et al. Epidemiology of fracture nonunion in 18 human bones. JAMA Surg 151, e162775 (2016).
Azi, M. L. et al. Autologous bone graft in the treatment of post-traumatic bone defects: a systematic review and meta-analysis. BMC Musculoskelet. Disord. 17, 1–10 (2016).
Schmidt, A. H. Autologous bone graft: Is it still the gold standard? Injury 52, S18–S22 (2021).
Finkemeier, C. G. Bone-grafting and bone-graft substitutes. J. Bone Joint. Surg. Am. 84, 454–464 (2002).
Jones, A. L. et al. Recombinant human BMP-2 and allograft compared with autogenous bone graft for reconstruction of diaphyseal tibial fractures with cortical defects. A randomized, controlled trial. J. Bone Joint Surg. Am. 88, 1431–1441 (2006).
Wang, E. A. et al. Recombinant human bone morphogenetic protein induces bone formation. Proc. Natl Acad. Sci. USA 87, 2220–2224 (1990).
Kirker-Head, C. A. Potential applications and delivery strategies for bone morphogenetic proteins. Adv. Drug Deliv. Rev. 43, 65–92 (2000).
Li, R. H. & Wozney, J. M. Delivering on the promise of bone morphogenetic proteins. Trends Biotechnol. 19, 255–265 (2001).
Babensee, J. E., McIntire, L. V. & Mikos, A. G. Growth factor delivery for tissue engineering. Pharm. Res. 17, 497–504 (2000).
Geiger, M., Li, R. H. & Friess, W. Collagen sponges for bone regeneration with rhBMP-2. Adv. Drug Deliv. Rev. 55, 1613–1629 (2003).
Epstein, N. E. & Schwall, G. S. Costs and frequency of ‘off-label’ use of INFUSE for spinal fusions at one institution in 2010. Surg. Neurol. Int. 2, 115 (2011).
Tannoury, C. A. & An, H. S. Complications with the use of bone morphogenetic protein 2 (BMP-2) in spine surgery. Spine J. 14, 552–559 (2014).
Epstein, N. Pros, cons, and costs of INFUSE in spinal surgery. Surg. Neurol. Int. 2, 10 (2011).
King, W. J. & Krebsbach, P. H. Growth factor delivery: how surface interactions modulate release in vitro and in vivo. Adv. Drug Deliv. Rev. 64, 1239–1256 (2012).
Lutolf, M. P. et al. Repair of bone defects using synthetic mimetics of collagenous extracellular matrices. Nat. Biotechnol. 21, 513–518 (2003).
Badylak, S. F., Freytes, D. O. & Gilbert, T. W. Extracellular matrix as a biological scaffold material: structure and function. Acta Biomater. 5, 1–13 (2009).
Mumcuoglu, D., Siverino, C., Tabisz, B., Kluijtmans, B. & Nickel, J. How to use BMP-2 for clinical applications? A review on pros and cons of existing delivery strategies. J. Transl. Sci. 3, 1–11 (2017).
Steen Redeker, E. et al. Protein engineering for directed immobilization. Bioconjug Chem 24, 1761–1777 (2013).
Bougioukli, S. et al. Ex vivo gene therapy using human bone marrow cells overexpressing BMP-2: “Next-day” gene therapy versus standard “two-step” approach. Bone 128, 115032 (2019).
Duchamp De Lageneste, O. et al. Periosteum contains skeletal stem cells with high bone regenerative potential controlled by Periostin. Nat. Commun. 9, 773 (2018).
Colnot, C., Zhang, X. & Tate, M. L. K. Current insights on the regenerative potential of the periosteum: Molecular, cellular, and endogenous engineering approaches. J. Orthop. Res. 30, 1869–1878 (2012).
Dwek, J. R. The periosteum: what is it, where is it, and what mimics it in its absence? Skeletal Radiol. 39, 319–323 (2010).
Ito, Y. et al. Localization of chondrocyte precursors in periosteum. Osteoarthr. Cartil. 9, 215–223 (2001).
Patro, B. P. et al. Traumatized periosteum: Its histology, viability, and clinical significance. Orthop. Rev. 14, 30044 (2021).
Muinos-López, E. et al. Hypoxia and reactive oxygen species homeostasis in mesenchymal progenitor cells define a molecular mechanism for fracture nonunion. Stem Cells 34, 2342–2353 (2016).
Karaoglu, S., Baktir, A., Kabak, S. & Arasi, H. Experimental repair of segmental bone defects in rabbits by demineralized allograft covered by free autogenous periosteum. Injury 33, 679–683 (2002).
Kanou, M. et al. Osteogenic potential of primed periosteum graft in the rat calvarial model. Ann. Plast. Surg. 54, 71–78 (2005).
Zhang, W. et al. Periosteum and development of the tissue-engineered periosteum for guided bone regeneration. J. Orthop. Transl. 33, 41–54, (2022).
Cheng, W. X. et al. PLGA/β-TCP composite scaffold incorporating cucurbitacin B promotes bone regeneration by inducing angiogenesis. J. Orthop. Transl. 31, 41–51 (2021).
Hoffman, M. D., Xie, C., Zhang, X. & Benoit, D. S. W. The effect of mesenchymal stem cells delivered via hydrogel-based tissue engineered periosteum on bone allograft healing. Biomaterials 34, 8887–8898 (2013).
Giannoudis, P. V., Harwood, P. J., Tosounidis, T. & Kanakaris, N. K. Restoration of long bone defects treated with the induced membrane technique: protocol and outcomes. Injury 47, S53–S61 (2016).
Llopis-Hernández, V. et al. Material-driven fibronectin assembly for high-efficiency presentation of growth factors. Sci. Adv. 2, e1600188 (2016).
Backes, E. H. et al. Polycaprolactone usage in additive manufacturing strategies for tissue engineering applications: a review. J. Biomed. Mater. Res. B Appl. Biomater. 110, 1479–1503 (2022).
Yang, X., Wang, Y., Zhou, Y., Chen, J. & Wan, Q. The application of polycaprolactone in three-dimensional printing scaffolds for bone tissue engineering. Polymers 13, 2754 (2021).
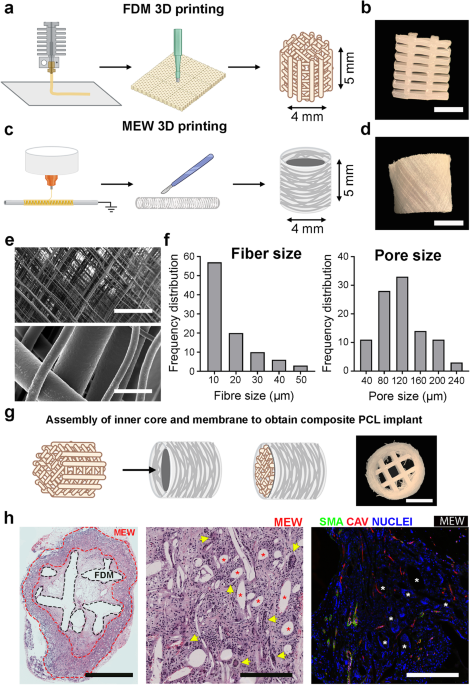
Baldwin, J. G. et al. Periosteum tissue engineering in an orthotopic in vivo platform. Biomaterials 121, 193–204 (2017).
Ramirez, M. I. et al. The alpha-isoform of caveolin-1 is a marker of vasculogenesis in early lung development. J. Histochem. Cytochem. 50, 33–42 (2002).
Mazo, M. et al. Transplantation of mesenchymal stem cells exerts a greater long-term effect than bone marrow mononuclear cells in a chronic myocardial infarction model in rat. Cell Transplant. 19, 313–328 (2010).
Gavira, J. J. et al. Repeated implantation of skeletal myoblast in a swine model of chronic myocardial infarction. Eur. Heart J. 31, 1013–1021 (2010).
Markova, V. et al. Endothelial cell markers are inferior to vascular smooth muscle cells markers in staining vasa vasorum and are non-specific for distinct endothelial cell lineages in clinical samples. Int. J. Mol. Sci. 24, 1959 (2023).
González‐Gil, A. B. et al. Periosteum-derived mesenchymal progenitor cells in engineered implants promote fracture healing in a critical-size defect rat model. J. Tissue Eng. Regen. Med. 13, 742–752 (2019).
Alford, A. I., Nicolaou, D., Hake, M. & McBride-Gagyi, S. Masquelet’s induced membrane technique: review of current concepts and future directions. J. Orthop. Res. 39, 707–718 (2021).
Cheng, Z. A. et al. Nanoscale coatings for ultralow dose BMP-2-driven regeneration of critical-sized bone defects. Adv. Sci. 6, 1800361 (2018).
Alba-Perez, A., Jayawarna, V., Childs, P. G., Dalby, M. J. & Salmeron-Sanchez, M. Plasma polymerised nanoscale coatings of controlled thickness for efficient solid-phase presentation of growth factors. Mater. Sci. Eng. C Mater. Biol. Appl. 113, 110966 (2020).
Granero-Molto, F., Weis, J. A., Longobardi, L. & Spagnoli, A. Role of mesenchymal stem cells in regenerative medicine: application to bone and cartilage repair. Expert Opin. Biol. Ther. 8, 255–68 (2008).
Granero-Moltó, F. et al. Mesenchymal stem cells expressing insulin-like growth factor-I (MSC IGF) promote fracture healing and restore new bone formation in irs1 knockout mice: analyses of MSC IGF autocrine and paracrine regenerative effects. Stem Cells 29, 1537–1548 (2011).
González-Gil, A. B. et al. Periosteum-derived mesenchymal progenitor cells in engineered implants promote fracture healing in a critical-size defect rat model. J. Tissue Eng. Regen. Med. https://doi.org/10.1002/term.2821 (2019).
Hornicek, F. J. et al. Factors affecting nonunion of the allograft-host junction. Clin. Orthop. Relat. Res. 382, 87–98 (2001).
Pearson, R. G., Bhandari, R., Quirk, R. A. & Shakesheff, K. M. Recent advances in tissue engineering. J. Long Term Eff. Med. Implants 27, 199–232 (2017).
Hu, J. & Ma, P. X. Nano-fibrous tissue engineering scaffolds capable of growth factor delivery. Pharm. Res. 28, 1273–1281 (2011).
Shastri, V. P. In vivo engineering of tissues: biological considerations, challenges, strategies, and future directions. Adv. Mater. 21, 3246–3254 (2009).
Yang, G. et al. Bioinspired membrane provides periosteum-mimetic microenvironment for accelerating vascularized bone regeneration. Biomaterials 268, 120561 (2021).
Roberts, S. J., van Gastel, N., Carmeliet, G. & Luyten, F. P. Uncovering the periosteum for skeletal regeneration: the stem cell that lies beneath. Bone 70, 10–18 (2015).
Lin, Z., Fateh, A., Salem, D. M. & Intini, G. Periosteum: biology and applications in craniofacial bone regeneration. J. Dent. Res. 93, 109–116 (2014).
Tsuji, K. et al. BMP2 activity, although dispensable for bone formation, is required for the initiation of fracture healing. Nat. Genet. 38, 1424–1429 (2006).
Li, Y., Hoffman, M. D. & Benoit, D. S. W. Matrix metalloproteinase (MMP)-degradable tissue engineered periosteum coordinates allograft healing via early stage recruitment and support of host neurovasculature. Biomaterials 268, 120535 (2021).
Zhuang, Z. et al. Periosteum mimetic coating on structural bone allografts via electrospray deposition enhances repair and reconstruction of segmental defects. ACS Biomater. Sci. Eng. 6, 6241–6252 (2020).
Al Hosni, R. et al. Mapping human serum–induced gene networks as a basis for the creation of biomimetic periosteum for bone repair. Cytotherapy 22, 424–435 (2020).
Moore, S. R. et al. Translating periosteum’s regenerative power: insights from quantitative analysis of tissue genesis with a periosteum substitute implant. Stem Cells Transl. Med. 5, 1739–1749 (2016).
Yu, Y. et al. Biomimetic periosteum-bone substitute composed of preosteoblast-derived matrix and hydrogel for large segmental bone defect repair. Acta Biomater. 113, 317–327 (2020).
Gupta, S. et al. Periosteum-mimicking tissue-engineered composite for treating periosteum damage in critical-sized bone defects. Biomacromolecules 22, 3237–3250 (2021).
Wunner, F. M. et al. Melt electrospinning writing of three-dimensional poly(ε-caprolactone) scaffolds with controllable morphologies for tissue engineering applications. J. Vis. Exp. 2017, 56289 (2017).
Filipowska, J., Tomaszewski, K. A., Niedźwiedzki, Ł., Walocha, J. A. & Niedźwiedzki, T. The role of vasculature in bone development, regeneration and proper systemic functioning. Angiogenesis 20, 291–302 (2017).
Gruber, H. E. et al. Genomewide molecular and biologic characterization of biomembrane formation adjacent to a methacrylate spacer in the rat femoral segmental defect model. J. Orthop. Trauma 27, 290–297 (2013).
Henrich, D. et al. Establishment and characterization of the Masquelet induced membrane technique in a rat femur critical-sized defect model. J. Tissue Eng. Regen. Med. 10, E382–E396 (2016).
Masquelet, A. C. The evolution of the induced membrane technique. Curr. Stat. Fut. Dir. 31, 3–8 (2016).
Pelissier, P., Masquelet, A. C., Bareille, R., Mathoulin Pelissier, S. & Amedee, J. Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J. Orthop. Res. 22, 73–79 (2004).
Gouron, R. et al. Osteoclasts and their precursors are present in the induced-membrane during bone reconstruction using the Masquelet technique. J. Tissue Eng. Regen. Med. 11, 382–389 (2017).
Nau, C. et al. Influence of the induced membrane filled with syngeneic bone and regenerative cells on bone healing in a critical size defect model of the rat’s femur. Injury 49, 1721–1731 (2018).
Tang, Q. et al. Masquelet’s induced membrane promotes the osteogenic differentiation of bone marrow mesenchymal stem cells by activating the Smad and MAPK pathways. Am. J. Transl. Res. 10, 1211 (2018).
Reddi, A. H. & Cunningham, N. S. Initiation and promotion of bone differentiation by bone morphogenetic proteins. J. Bone Min. Res. 8, S499–S502 (1993).
Dumic-Cule, I. et al. Bone morphogenetic proteins in fracture repair. Int. Orthop. 42, 2619–2626 (2018).
Mizrahi, O. et al. BMP-6 is more efficient in bone formation than BMP-2 when overexpressed in mesenchymal stem cells. Gene Therapy 20, 370–377 (2012). 20:4.
Zhu, L. et al. Application of BMP in bone tissue engineering. Front. Bioeng. Biotechnol. 10, 402 (2022).
Zara, J. N. et al. High doses of bone morphogenetic protein 2 induce structurally abnormal bone and inflammation in vivo. Tissue Eng. Part A 17, 1389–1399 (2011).
James, A. W. et al. A review of the clinical side effects of bone morphogenetic protein-2. Tissue Eng. Part B Rev. 22, 284–297 (2016).
AW, Y. et al. The healing of segmental bone defects, induced by recombinant human bone morphogenetic protein (rhBMP-2). A radiographic, histological, and biomechanical study in rats. J. Bone Joint Surg. Am. 74, 535–537 (1992).
Kim, I. S. et al. Promising efficacy of Escherichia coli recombinant human bone morphogenetic protein-2 in collagen sponge for ectopic and orthotopic bone formation and comparison with mammalian cell recombinant human bone morphogenetic protein-2. Tissue Eng. Part A 17, 337–348 (2011).
Stuckensen, K. et al. Anisotropic cryostructured collagen scaffolds for efficient delivery of RhBMP-2 and enhanced bone regeneration. Materials 12, 3105 (2019).
Mumcuoglu, D. et al. Injectable BMP-2 delivery system based on collagen-derived microspheres and alginate induced bone formation in a time-and dose-dependent manner. Eur. Cell Mater. 35, 242–254 (2018).
Boerckel, J. D. et al. Effects of protein dose and delivery system on BMP-mediated bone regeneration. Biomaterials 32, 5241–5251 (2011).
Araña, M. et al. Epicardial delivery of collagen patches with adipose-derived stem cells in rat and minipig models of chronic myocardial infarction. Biomaterials 35, 143–151 (2014).
Lois, C., Hong, E. J., Pease, S., Brown, E. J. & Baltimore, D. Germline transmission and tissue-specific expression of transgenes delivered by lentiviral vectors. Science 295, 868–872 (2002).
- SEO Powered Content & PR Distribution. Get Amplified Today.
- PlatoData.Network Vertical Generative Ai. Empower Yourself. Access Here.
- PlatoAiStream. Web3 Intelligence. Knowledge Amplified. Access Here.
- PlatoESG. Carbon, CleanTech, Energy, Environment, Solar, Waste Management. Access Here.
- PlatoHealth. Biotech and Clinical Trials Intelligence. Access Here.
- Source: https://www.nature.com/articles/s41536-023-00330-2



