Key Points
- Breast milk is the best source of nutrition for most infants. We do not know whether mothers with COVID-19 can transmit the virus via breast milk, but the limited data available suggest this is not likely to be a source of transmission.
- Whether and how to start or continue breastfeeding should be determined by the mother in coordination with her family and healthcare providers.
- A mother with confirmed COVID-19 should be counseled to take all possible precautions to avoid spreading the virus to her infant, including hand hygiene and wearing a cloth face covering.
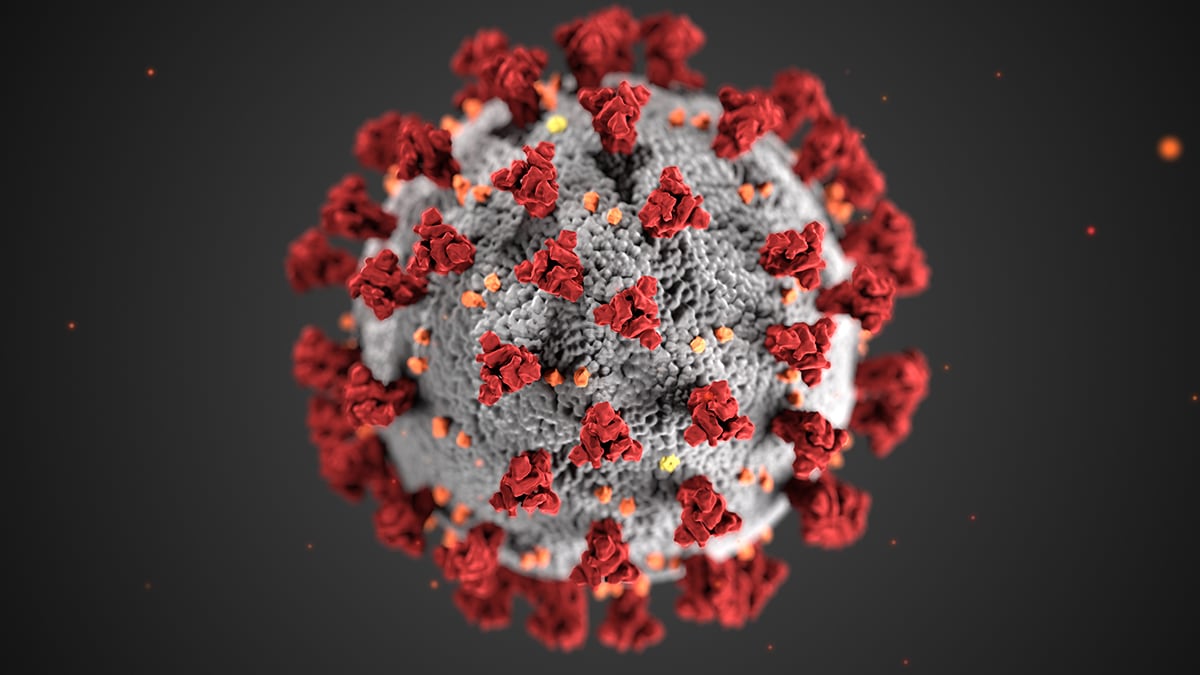
This interim guidance is intended for healthcare providers who care for breastfeeding women and infants who receive breast milk feeds in the context of coronavirus disease 2019 (COVID-19). This interim guidance is based on what is currently known about SARS-CoV-2, the virus that causes COVID-19, and the transmission of other viral respiratory pathogens. CDC will update this interim guidance as additional information becomes available. For breastfeeding guidance in the immediate postpartum setting, refer to Considerations for Inpatient Obstetric Healthcare Settings.
Transmission of SARS-CoV-2 through breast milk
These considerations are based upon the limited evidence available to date about transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19, and knowledge of other viruses that cause severe respiratory illness including influenza and severe acute respiratory syndrome coronavirus (SARS-CoV).
Breast milk is the best source of nutrition for most infants, and it provides protection against many illnesses. There are rare exceptions when breastfeeding or feeding expressed breast milk is not recommended. We do not know whether mothers with COVID-19 can transmit the virus via breast milk, but the limited data available suggest this is not likely to be a source of transmission.
Pasteurized donor human milk is important in the care of preterm infants. No information is currently available regarding the effect of pasteurization on SARS-CoV-2 but similar viruses are inactivated with this process. Disruptions in human milk donations may be seen during the COVID-19 pandemic. If hospitals have difficulty acquiring donor human milk, available supplies should be prioritized for preterm infants who will benefit most from human milk feeds.
Guidance on breastfeeding for mothers in the context of COVID-19
Whether and how to start or continue breastfeeding should be determined by the mother, in coordination with her family and healthcare providers.
A mother with suspected, probable, or confirmed COVID-19 should be counseled to take all possible precautions to avoid spreading the virus to her infant. She should be instructed to wash her hands using soap and water, especially if her hands are visibly soiled, before touching the infant. If soap and water are not available, she should use a hand sanitizer with at least 60% alcohol. Additionally, mothers should wear a cloth face covering while feeding at the breast. If expressing breast milk either by hand expression or with a breast pump, the mother should clean her hands, as instructed above, before touching any pump or bottle parts and wear a cloth face covering. Mothers should be educated about recommendations on how to properly clean and sanitize breast pumps. If possible, expressed breast milk should be fed to the infant by a healthy caregiver, who is not at high-risk for severe illness from COVID-19.
Breastfeeding mothers who work in settings with higher risk of potential exposure to SARS-CoV-2, such as healthcare personnel and first responders, may have additional concerns related to expression of breast milk while at work. These mothers should follow the same recommendations outlined above given they may be at higher risk of infection with SARS-CoV-2. Ideally, employers would provide breastfeeding employees with a private, non-bathroom space for milk expression. Additional information for healthcare personnel, including those who are pregnant, have underlying medical conditions, or who are living with someone who is at risk for severe illness from COVID-19, is available.
There is evidence that SARS-CoV-2 remains on surfaces for several hours to days. Healthcare providers should discuss a mother’s individual circumstances (e.g., level of exposure to persons with suspected or confirmed COVID-19, availability and proper use of personal protective equipment) when counseling the mother about additional precautions prior to breastfeeding or expression of breast milk while at work. Currently, there is a lack of evidence to support precautions such as cleansing the breast prior to breastfeeding or milk expression, or disinfecting external surfaces of milk collection devices (e.g., bottles, milk bags), as steps to reduce potential transmission of SARS-CoV-2. Mothers may consider additional steps such as these to minimize theoretic potential routes of exposure. Additional information on disinfecting facilities, such as workplace lactation rooms, is available.
Breastfed infants of women with confirmed COVID-19
An infant being breastfed by a mother who is confirmed to have COVID-19 should be considered as having suspected COVID-19 for the purposes of infection control and prevention for the duration of the mother’s recommended period of home isolation and 14 days thereafter. The same approach should be taken with respect to an infant who has any other ongoing, close contact with another person who has confirmed COVID-19. Mothers should be counseled to inform their child’s healthcare provider that their child has had high-risk contact with a person confirmed to have COVID-19.
Well child checks and lactation services
Healthcare providers are encouraged to prioritize newborn care and vaccination of infants and young children (through 24 months of age) when possible. Given the potential challenges related to breastfeeding in the context of COVID-19, the need for weight checks and visual or laboratory assessment for jaundice, and the stressors of social distancing, every effort should be made to conduct newborn follow-up visits in person. Healthcare providers should consider how to minimize exposure to the SARS-CoV-2 virus for patients, caregivers, and staff in the context of their local COVID-19 epidemiology and practice environment. Additional information on infection prevention and control in the healthcare setting is available.
Alternative approaches, such as telemedicine, may be considered when providing lactation support services to breastfeeding dyads. Lactation service providers who must see a mother or infant with suspected or confirmed COVID-19 should follow recommended infection prevention and control measures, including the use of recommended personal protective equipment (PPE). If no PPE is available, then lactation service providers should carefully consider if alternative approaches will reduce the risk of exposure for the lactation service provider and are safe for care of the breastfeeding dyad.
Source: https://tools.cdc.gov/api/embed/downloader/download.asp?m=403372&c=406649



